The success of CAR T-Cells has highlighted two things – one, that immunotherapy should be regarded as one of the essential treatment strategies for cancer, and two, although there are reports of adverse effects of CAR T therapy in certain patients during the 2016 clinical trials, the possibility of adverse events with it is much lower than that with other treatment methods, e.g. chemotherapy and radiation. In August 2017, Novartis made news with the USFDA approval of Kymriah, the first ever chimeric antigen receptor (CAR) T-cells therapy for B-cell acute lymphoblastic leukaemia (ALL). This therapy is meant for patients with refractory or relapsing leukaemia in the ages of 0 to 25 years. This development became significant because it sparked some big billion investments in immunotherapy research.
As is widely known, malignancies are usually removed from the human body using surgery, chemotherapy and radiation in a planned span of time, based on the patient’s age, immunity and metabolic status parameters. However, in more than 60% of cancer cases, even after the third line of treatment i.e. chemotherapy or radiation therapy, small masses of neoplasms remain inside, due to resistance to treatment processes, chemotherapeutic drugs, or locational attributes. These refractory cancer cells may grow in size and re-emerge again, as what is known as relapsing cancer and is most often non-treatable and risky. Gene-editing on T cells has shown a good positive outcome rate in Phase I to III clinical trials, up to the extent that now immunotherapy is considered as the ‘Fifth Pillar’ of treating malignancies.
Belief in CAR T-Cells’ Innate Potential
The interest in developing the body’s immunity system and harnessing its potential to fight cancer cells has been around among immunologists since the first incidence of unspecified neoplasms. The earliest existing immunology studies conducted by clinicians and pathologists have tested basic cell engineering strategies in bacterial cells in order to use them as potential antigens inside the human body. A surgeon, Dr William Coley inserted cultured streptococcus into a patient’s bone cancer cells in 1893 that shrunk cancer in size. In this scenario, the bacterial genome triggers the patient’s immunity system to sense cancer cells and diminish their size or kill them via necrosis. Another noted immunologist in Israel, Zelig Eshhar, first reported the successful expression of CARs on the surface of T cells in 1993.
But the previous decade and a half showed immunology researchers only closed doors, plagued with funding limitations and a lack of infrastructure. With minimal resources at hand, Dr Carl June, one of the most potent immunologists at the University of Pennsylvania, continued his work on developing genetically engineered T-cells. Progress was slow for the most part, yet he was able to publish his findings as case studies until, in 2010, 5-year-old Emily Whitehead with B-cell ALL landed at the University of Pennsylvania after refusing to take hospice for her unstoppable leukaemia. Her enrollment in a CART-19 clinical trial and the subsequent successful ALL remission was a victory not just for her cancer but for the immunologists at UPenn as well. Beside the progress with stem cells treatments, gene-editing based cell therapies started becoming the focal points of cancer research.

Image source – EMBO Molecular Medicine Journal. Title – Clinical development of CAR T-cells—challenges and opportunities in translating innovative treatment concepts. Jessica Hartmann et al. (2017)
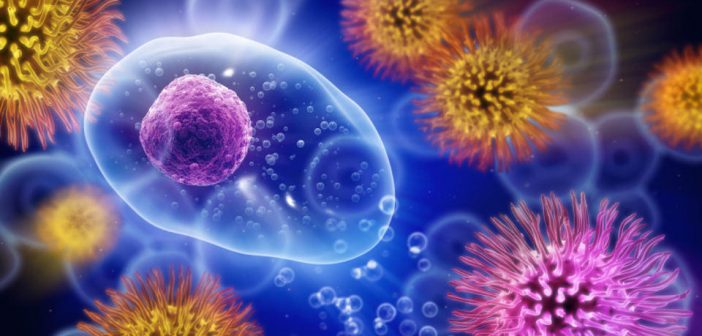
The basic units of the innate immunity system, T Cells, are re-engineered with chimeric antigen receptors (CARs), which are surface-expressed recombinant structures with the immunotherapy drug inside them. The re-engineered T cells grow inside the body, detect cancer cells and kill them. CAR T-cells, as they are hugely called, are capable of self-proliferation and self-activation, with each generation of cells expressing highly reactive cancer-killing molecules. These are single-chain variable fragments which proliferate immediately and organise themselves according to different tumor-antigen specificities. They are connected via cell-surface receptors to signalling domains on the mature T cells that control their growth and ligand-binding specificities.
Administering CAR T therapy carries with it a preferential list of indications, governed by the rate of disease progression and patient’s pre-conditioning. As with other oncologic treatment side effects, CAR T-cells therapy is used to administer Actembra for the treatment of Cytokine-release-syndrome, which occurs as a side-effect after treatment with Kymriah. So, long story short, in future, when patients undergo treatment for B-cell ALL, chances are patients will be requiring Actemra as well. Maybe, future research on CAR T-cell therapy can be focussed on delivering combination drugs as well.
Why CAR T Therapy is Big For Cancer
T Cells expressing novel Chimeric Antigen Receptors are not new, but the breakthrough with 3 significant immunotherapy drug approvals has raised the promise for Biotech companies to test its efficacy in Melanomas, Lymphomas and Leukaemias. Academic researchers have even started evaluating CAR T Cells for solid tumours in the pancreas, intestines and liver. This is a remarkable extrapolation to consider, since every new gene therapy, using DNA editing, recombinant structures, protein expression or novel drug carrier undergoes a long haul of trials to get them approved for larger use.
It’s no surprise that almost a century of research work has been spent on cancer to conclude only a few specific cancer types as actually treatable or more manageable. Thus, the final outcomes of these novel therapies strike a difference, and the technology of gene-edited T Cells fighting hematologic cancers is a big breakthrough to consider. CAR T-cells therapy has broken longstanding barriers in therapeutic research with recent reports of acceptable safety profiles that can be used to increase cancer survival rates. Even till a few months ago, research work was more focussed on cellular biomarkers, protein biomarkers or other agents that helped in diagnosing cancer as much as possible. But now scientists are exploring better ways to manage secondary lines of treatments for masses or lesions that have undergone radiation therapy or chemotherapy.
This breakthrough, in itself, is a big impetus to cancer research and got companies like Juno Therapeutics, Gilead, Becton Dickinson, Innate Pharma and Fierce Biotech to invest in immunotherapies. Gilead’s announcement in October about its $11.9 Bn acquisition of Kite Pharma and the subsequent FDA approval of Yescarta for adult refractory large B-cell lymphoma is a big indication of this massive shift.
CAR T-Cells Opened The Door For More Drugs
After Novartis’ Tisagenlecleucel (Kymriah) received FDA-approval this year, more immunotherapy drug approvals followed. An important one being Yescarta (generic name – Axicabtagene ciloleucel) for the treatment of relapsed or refractory large B-cell lymphoma in patients who underwent 2 or more lines of prior oncologic treatment. Further testing of Yescarta for systemic cancers as well as other B-cell lymphomas are underway, including high-grade B-cell lymphoma and primary mediastinal large B-cell lymphoma.
The other drug that received FDA approval is Actemra (generic name – Tocilizumab) that is used to mitigate the possible side effects of receiving immunotherapeutic drugs and induced T-cell activation. These developments also point to the fact that when patients are due for treatment with CAR-T cells, they are required to undergo a conditional chemotherapy in some cases which takes care of chemotherapy-resistance.
Until now, 89 clinical trials have been conducted in various countries, with China leading the way (66 CAR T clinical trials) and European Biotechnology labs fast catching up (14 CAR T Clinical trials). Every day, new data from studies on investigating CAR T-cells for stomach cancers, liver cancers, solid tumours in ovaries are being published. However, the toxicity indications and long-term costs of developing the therapy remain tough challenges to overcome. The toxicity studies have been reported in a few patients who enrolled for Phase I & II trials, but the infrastructure to manage clinical emergencies arising in patients receiving T Cell therapy have to improve.
CAR T Cells Demonstrate High Response Rates in Relapsed and Refractory NHL #TcellRx #sehhseth17 #lymsm pic.twitter.com/BggEv4T5wS
— Miguel Perales M.D. (@DrMiguelPerales) October 25, 2017
Clinical trials for testing toxicity ratios of CAR T Cells are underway since 2015, mostly investigational and observational stages as oncologists say that understanding the toxicity component of T Cells therapy is a long drawn process. What is important to note here is, CRISPR edited gene fragments are used for re-engineering T Cells and these fragments don’t show any damage or overstimulation effects in the initial growth stages. But the expression of immunity molecules like interleukins and cytokines even if considered as unsolicited is still not worth putting a stop too. Interleukins and Cytokines are the T Cells naturally expressed chemicals.
Another key area of research with CAR T-cells is to study its maturation stages in order to determine the correct stage of its interaction with tumour-specific antigens. In the case of B-cell lymphomas, scientists are trying to single out even better target strategies so that the life of healthy B Cells is the least compromised. Much work remains to be done on CAR T-cells to check if other targeted therapies like Gleevec (Imatinib), Herceptin (Trastuzumab) or Actembra (Tocilizumab) can be combined together for more effective anti-tumour drugs.
————
Want to consult an immunotherapy specialist? Get in touch with an expert on Kolabtree.





1 Comment
Great article. Controlling the side effects of T Cell Therapy & building awareness of the potential to fight cancer is an interesting conversation.